Ankylosing Spondylitis
Ankylosing Spondylitis (AS) is a chronic inflammatory arthritis that mainly affects the spine, causing pain, stiffness, and reduced flexibility. Over time, spinal bones may fuse, leading to decreased mobility and a forward-curved posture. Although it is a lifelong condition, early diagnosis and proper management can help control symptoms and maintain quality of life.
-
Chronic back pain and stiffness, especially in the lower back and hips
Pain that improves with movement but worsens with rest
Morning stiffness lasting longer than 30 minutes
Fatigue
Reduced flexibility in the spine
Pain in other joints (like shoulders, hips, knees)
In advanced cases, forward curvature of the spine (hunched posture)
Eye inflammation (uveitis), causing eye pain and blurred vision (in some people)
-
Medical history (asking about back pain, stiffness, and family history)
Physical examination (checking spine flexibility and posture)
Imaging tests:
X-rays to look for changes in the sacroiliac joints and spine
MRI to detect early inflammation before X-rays show damage
Blood tests:
Testing for the HLA-B27 gene, which is linked to a higher risk of AS
Inflammatory markers like CRP and ESR
-
Medications: NSAIDs, TNF inhibitors, and IL-17 inhibitors to control inflammation.
Exercise & Physical Therapy: Key to maintaining posture and flexibility.
Lifestyle Changes: Regular activity, good posture, and avoiding smoking.
Surgery: Rarely needed, for severe joint or spinal issues.
Regular Monitoring: Ongoing care with a rheumatologist to adjust treatment as needed.

Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (CFS), or ME/CFS, is a long-term illness marked by extreme, unrelenting fatigue that isn't relieved by rest. It can severely impact daily life and involve various physical and mental symptoms. Though complex and often misunderstood, proper support and management can help improve quality of life.
-
Extreme, unexplained fatigue that doesn't improve with rest
Post-exertional malaise (worsening symptoms after physical or mental activity)
Sleep disturbances (trouble falling or staying asleep)
Muscle or joint pain without swelling or redness
Memory or concentration issues (“brain fog”)
Frequent sore throats, headaches, or enlarged lymph nodes
Dizziness or feeling faint when standing
-
Medical history review and symptom assessment
Excluding other possible conditions (like thyroid issues, anemia, or depression)
Meeting specific diagnostic criteria (such as fatigue lasting longer than six months, post-exertional malaise, and unrefreshing sleep). Some tests may be done to rule out other illnesses.
-
There is no cure, but treatment focuses on symptom relief and energy management:
Pacing: Balance activity and rest to avoid crashes.
Sleep support: Improve sleep with good habits or therapy.
Pain management: Use appropriate medications for pain and other symptoms.
Cognitive support: Address brain fog and emotional health.
Treat related conditions: Manage overlapping issues like anxiety, IBS, or fibromyalgia.
Lifestyle care: Gentle movement, stress reduction, and nutrition.

Enteropathic Arthritis
Enteropathic Arthritis is a type of inflammatory arthritis that occurs in people with inflammatory bowel diseases (IBD), like Crohn’s disease or ulcerative colitis. It causes joint pain, swelling, and stiffness, especially in the spine and large joints like knees and ankles. The inflammation is linked to the immune system's reaction to intestinal disease, and symptoms can flare with gut symptoms.
-
Joint pain, swelling, and stiffness (knees, ankles, hips)
Lower back pain, especially in the morning
Fatigue
Gut symptoms like diarrhea, abdominal pain, or cramping
Eye inflammation (redness, pain, blurred vision)
Skin issues like rashes
-
Medical history (IBD diagnosis or symptoms)
Physical examination of joints and spine
Blood tests to check for inflammation markers
Imaging tests (X-rays, MRI) to detect joint damage
Stool tests to assess bowel inflammation
-
Anti-inflammatory medications (NSAIDs): Used cautiously, as they can worsen IBD.
Steroids: Help control inflammation in both joints and the gut short term.
DMARDs: Like methotrexate or sulfasalazine for ongoing joint symptoms.
Biologics: TNF inhibitors (e.g., infliximab, adalimumab) treat both arthritis and IBD.
Lifestyle support: Includes physical therapy, joint-friendly exercise, and managing IBD through diet and stress reduction.

Fibromyalgia
Fibromyalgia is a long-term (chronic) disorder that causes widespread pain, tenderness, fatigue, and other symptoms throughout the body. It affects how the brain and spinal cord process pain signals, making even mild pressure feel painful. Fibromyalgia can make everyday activities harder, but with the right care and support, symptoms can be managed successfully.
-
Widespread muscle pain and tenderness
Chronic fatigue — feeling tired even after sleeping
Memory and concentration problems ("fibro fog")
Headaches and migraines
Sleep disturbances
Irritable bowel syndrome (IBS) symptoms (like bloating or diarrhea)
Depression or anxiety
-
Reviewing symptoms and medical history
Physical exam to check for tender points
Excluding other conditions like arthritis or thyroid issues (since fibromyalgia doesn’t cause visible inflammation or joint damage)
Doctors often use criteria such as how widespread the pain is and how long symptoms have lasted (usually 3+ months).
-
Treatment includes medications (pain relievers, antidepressants, nerve pain drugs), regular low-impact exercise, better sleep habits, stress management, and cognitive therapy. The goal is to reduce symptoms and improve daily function.

Gout
Gout is a common form of inflammatory arthritis that causes sudden, intense pain, swelling, and redness, usually in one joint at a time. It happens when uric acid builds up in the blood and forms sharp crystals in the joints, leading to painful flare-ups. Gout most often affects the big toe, but it can also affect the ankles, knees, wrists, and fingers.
-
Sudden, severe joint pain (often starting at night)
Swelling and redness around the affected joint
Warmth and tenderness at the joint
Limited joint movement during and after a flare
Lingering discomfort even after the worst of the pain subsides
-
Medical history and asking about symptoms
Physical examination of the affected joint
Joint fluid analysis (removing fluid from the joint to look for uric acid crystals)
Blood tests to check uric acid levels
Imaging tests like ultrasound or X-rays to detect joint damage or uric acid crystal deposits
-
Acute attacks: NSAIDs, colchicine, or corticosteroids to reduce pain and inflammation.
Long-term management: Medications like allopurinol or febuxostat to lower uric acid levels.
Lifestyle changes: Limit alcohol, red meat, and sugary foods; stay hydrated; maintain a healthy weight.

Juvenile Arthritis
Juvenile Arthritis (JA) is an umbrella term for types of arthritis that affect children under the age of 16. It happens when a child’s immune system mistakenly attacks healthy joints, causing inflammation, pain, and stiffness.
-
Joint pain, swelling, or stiffness, especially in the morning
Limping or difficulty using a limb
Fatigue or irritability
Fever and rash (especially with systemic JA)
Growth problems or uneven limb growth
Eye inflammation (uveitis) in some types
-
Detailed medical history and physical exam
Blood tests (like ANA, RF, ESR) to check for inflammation and autoantibodies
Imaging tests (X-rays, MRI, ultrasound) to look for joint damage
Eye exams to check for uveitis Diagnosis can be tricky since symptoms sometimes mimic other illnesses, making specialist care important.
-
Acute attacks: NSAIDs, colchicine, or corticosteroids to reduce pain and inflammation.
Long-term management: Medications like allopurinol or febuxostat to lower uric acid levels.
Lifestyle changes: Limit alcohol, red meat, and sugary foods; stay hydrated; maintain a healthy weight.

Lupus
Lupus (Systemic Lupus Erythematosus) is a chronic autoimmune disease where the immune system, which normally protects the body, mistakenly attacks healthy tissues. It can cause inflammation and damage to many parts of the body — including the skin, joints, kidneys, heart, lungs, and brain.
-
Fatigue (extreme tiredness) & Joint pain and swelling
Skin rashes, especially a butterfly-shaped rash over the cheeks and nose
Sensitivity to sunlight (skin rashes triggered by sun exposure)
Fever without a clear cause
Hair loss (thinning hair) & Mouth sores
Chest pain when breathing deeply (from lung or heart inflammation)
Swelling in legs or around eyes (possible kidney involvement)
Cognitive difficulties, like trouble focusing or memory problems
-
Medical history review (asking about symptoms and family history)
Physical examination (looking for rashes, joint swelling, and signs of organ involvement)
Blood tests used to diagnose and monitor lupus include the ANA test, which is usually positive in lupus patients, and more specific tests like anti-dsDNA and anti-Smith antibodies. A complete blood count (CBC) checks for anemia and low white cells or platelets. Kidney and liver function tests assess organ health, while ESR and CRP measure inflammation levels.
Imaging tests: X-rays or echocardiograms if lung or heart involvement is suspected.
-
Medications: NSAIDs for pain, antimalarials (like hydroxychloroquine) for disease control, corticosteroids for flares, and immunosuppressants or biologics for more severe cases.
Lifestyle: Sun protection, stress management, regular exercise, and a balanced diet.
Monitoring: Regular check-ups to track symptoms and organ function.

Mixed Connective Tissue Disease (MCTD)
Mixed Connective Tissue Disease (MCTD) is a rare autoimmune disorder that shows features of several diseases, including lupus, scleroderma, polymyositis, and sometimes rheumatoid arthritis. In MCTD, the immune system mistakenly attacks healthy tissues, leading to joint pain, muscle weakness, skin changes, and other systemic problems.
-
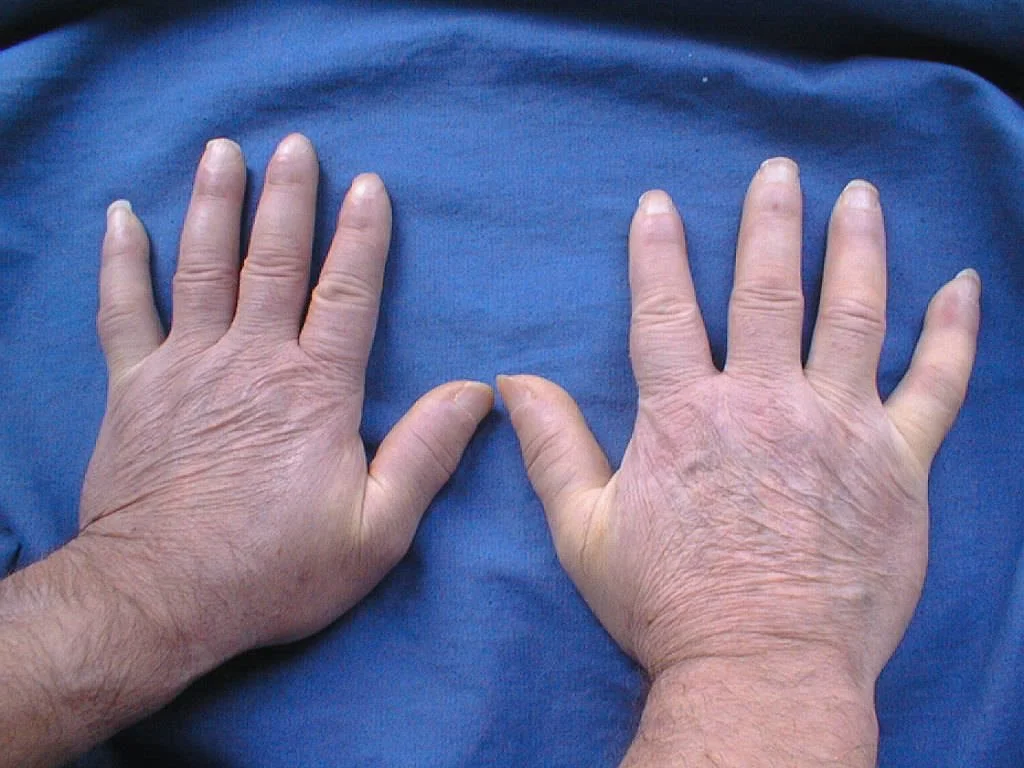
Swollen hands and fingers (“sausage digits”)
Joint pain and stiffness
Muscle weakness
Fatigue and low energy
Skin rashes or thickening
Raynaud’s phenomenon (fingers turning white or blue in the cold)
Difficulty swallowing or breathing
Pulmonary hypertension (high blood pressure in the lungs)
-
Blood tests to detect high levels of anti-RNP antibodies (specific to MCTD)
Physical examination to check for signs like joint swelling, muscle weakness, and skin changes
Imaging tests (X-rays, echocardiograms) to check for internal organ involvement
Excluding other autoimmune diseases by carefully assessing symptoms
-
Medications: NSAIDs for pain, corticosteroids for inflammation, and immunosuppressants (like methotrexate or azathioprine) for more severe symptoms.
Symptom-specific care: Treats related issues like Raynaud’s, lung involvement, or muscle weakness.
Lifestyle support: Includes regular exercise, a balanced diet, and avoiding cold exposure.

Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, caused by the gradual breakdown of cartilage — the smooth tissue that cushions joints. As the cartilage wears away, bones can rub against each other, leading to pain, swelling, stiffness, and reduced movement. Osteoarthritis can affect any joint, but it’s most common in the knees, hips, hands, and spine. It’s often called a "wear-and-tear" disease.
-
Joint pain that worsens with activity and eases with rest
Stiffness (especially in the morning or after sitting)
Swelling around the joints
Loss of flexibility or range of motion
A grating sensation when moving the joint (crepitus)
Bone spurs (extra bits of bone that feel like hard lumps under the skin)
-
Medical history (asking about joint symptoms, injuries, and family history)
Physical examination (checking for tenderness, swelling, and movement limitations)
Imaging tests:
X-rays to show cartilage loss, bone damage, or bone spurs
MRI (less common) for detailed images of joints and soft tissues
Lab tests:
Blood tests to rule out other types of arthritis (like rheumatoid arthritis)
Joint fluid analysis if the diagnosis isn’t clear
-
Medications: Pain relievers like acetaminophen, NSAIDs, and topical creams.
Exercise & Physical Therapy: To improve strength, flexibility, and joint function.
Lifestyle changes: Weight management, joint protection, and low-impact activity.
Supportive therapies: Braces, orthotics, or assistive devices if needed.
Surgery: Joint replacement in severe cases.
Lifestyle support: Includes regular exercise, a balanced diet, and avoiding cold exposure.

Polymyalgia Rheumatica
Polymyalgia Rheumatica (PMR) is an inflammatory disorder that causes widespread muscle pain and stiffness, especially in the shoulders, neck, and hips. It typically affects adults over the age of 50 and can develop suddenly. The inflammation is thought to be related to an overactive immune response. While PMR can cause significant discomfort, it usually responds well to proper treatment.
-
Aching and stiffness in the shoulders, neck, hips, and thighs
Morning stiffness lasting more than 30 minutes
Fatigue and low energy
Mild fever or feeling generally unwell
Weight loss
Limited range of motion
-
Physical examination checking for tenderness and stiffness
Blood tests to measure inflammation markers (like ESR and CRP)
Response to corticosteroids — often a dramatic improvement after starting steroids supports the diagnosis
Ruling out other conditions like rheumatoid arthritis, lupus, or infections
-
Corticosteroids: Low-dose prednisone is the main treatment, often leading to rapid symptom relief.
Gradual tapering: Steroid dose is slowly reduced over time to minimize side effects.
Monitoring: Regular check-ups to track symptoms, inflammation (ESR/CRP), and side effects.
Bone health support: Calcium, vitamin D, and sometimes bone-strengthening medications to prevent steroid-related bone loss.

Psoriatic Arthritis
Psoriatic Arthritis (PsA) is a chronic autoimmune disease that causes joint pain, swelling, and stiffness, often alongside psoriasis (a skin condition that causes red, scaly patches). In PsA, the immune system attacks healthy joints and skin, leading to inflammation and tissue damage over time.
-
Joint pain, swelling, and stiffness (especially in fingers, toes, knees, and ankles)
Back pain (if the spine is involved — called spondylitis)
Sausage-like swelling in fingers or toes (called dactylitis)
Skin rashes or scaly patches (typical of psoriasis)
Nail changes (pitting, thickening, or separation from the nail bed)
Fatigue
Eye inflammation (redness, pain — uveitis)
-
Medical history review (asking about psoriasis, joint issues, and family history)
Physical examination (checking joints, nails, skin, and spine)
Blood tests:
To check for inflammation (ESR, CRP)
To rule out other conditions like Rheumatoid Arthritis (RA factor, anti-CCP antibodies)
Imaging tests:
X-rays, MRI, or ultrasound to spot joint damage early
Skin and nail exam for signs of psoriasis
-
Medications: NSAIDs for pain, DMARDs (like methotrexate), and biologics (e.g., TNF or IL-17 inhibitors) to control inflammation and prevent joint damage.
Lifestyle: Regular exercise, healthy weight, and skin care.
Physical therapy: Improves joint function and mobility.
Monitoring: Regular follow-up to manage flares and adjust treatment.

Reactive Arthritis
Reactive Arthritis is a type of inflammatory arthritis that develops after an infection, usually in the urinary tract, intestines, or genitals. It causes joint pain and swelling, often in the knees, ankles, and feet. Reactive arthritis can also affect the eyes, skin, and urinary system. It is part of a group of conditions called “spondyloarthritis” and can happen to people of any age, often between the ages of 20–40.
-
Joint pain and swelling (especially knees, ankles, feet)
Lower back pain
Inflammation of the eyes (redness, pain)
Painful urination or urinary symptoms
Skin rashes or mouth ulcers
Swelling of fingers or toes ("sausage digits")
-
Medical history (including any recent infections)
Physical examination of joints, eyes, and skin
Blood tests to check for inflammation and infections
Urine or stool tests to identify infections
Imaging tests (X-rays or ultrasound) to look for joint inflammation
-
Antibiotics: If an infection is still present, especially for underlying bacterial causes.
NSAIDs: First-line treatment to reduce joint pain and inflammation.
Corticosteroids: For more severe or persistent joint symptoms.
DMARDs: Such as sulfasalazine or methotrexate for chronic or recurrent cases.
Physical therapy: Helps maintain joint mobility and muscle strength.

Scleroderma
Scleroderma, also known as Systemic Sclerosis, is a rare autoimmune disease that causes the skin and connective tissues to become thick and hard. It can also affect internal organs like the heart, lungs, kidneys, and digestive system. The disease happens when the body produces too much collagen, leading to tissue scarring and damage. Scleroderma can range from mild skin involvement to serious, life-threatening organ complications.
-
Thickening or tightening of the skin, especially on the fingers, hands, and face
Raynaud’s phenomenon (fingers and toes turning white or blue in the cold)
Joint pain and stiffness
Heartburn, difficulty swallowing, or digestive issues
Shortness of breath or dry cough (lung involvement)
Kidney problems
Fatigue and muscle weakness
-
Physical examination of the skin and joints
Blood tests to look for specific autoantibodies (like ANA, anti-Scl-70)
Pulmonary function tests to check lung health
Echocardiogram to assess heart involvement
Skin biopsy in some cases
Imaging tests (CT scan, X-rays) for internal organ assessment
-
No cure, but treatment focuses on managing symptoms and preventing complications.
Immunosuppressants, Such as methotrexate or mycophenolate for skin and lung involvement.
Blood pressure meds: Especially ACE inhibitors for kidney protection and Raynaud’s phenomenon.
Proton pump inhibitors (PPIs): For acid reflux and GI symptoms.
Physical therapy: To maintain joint flexibility and function.
Regular monitoring: To detect and manage organ involvement early.

Sjögren’s Syndrome
Sjögren’s Syndrome is a chronic autoimmune disease where the body’s immune system attacks the glands that produce moisture, like tears and saliva. This leads to dry eyes, dry mouth, and can also affect joints, skin, kidneys, lungs, and nerves.
-
Dry, gritty, or burning eyes
Dry mouth, trouble swallowing, or frequent dental cavities
Swelling in salivary glands (especially under the jaw)
Joint pain and stiffness
Fatigue and feeling run down
Skin dryness, rash, or numbness in the hands and feet
-
Medical history and symptom review
Blood tests for specific autoantibodies (like SSA/Ro and SSB/La)
Schirmer’s test to measure tear production
Salivary gland tests or biopsy
Eye exams to check for dryness and damage
-
Symptom relief: Artificial tears and saliva substitutes for dry eyes and mouth.
Medications: Pilocarpine or cevimeline to stimulate saliva/tear production; NSAIDs or hydroxychloroquine for joint pain and fatigue.
Immunosuppressants: For more severe systemic involvement (e.g., methotrexate or rituximab).
Dental and eye care: Regular check-ups to prevent complications like cavities or eye infections.
Lifestyle: Stay hydrated, avoid triggers like caffeine and alcohol, and use humidifiers.